TYPES OF BREAST CANCER
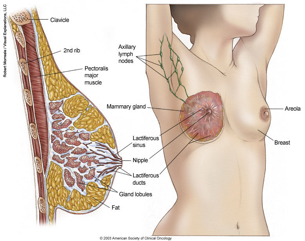
- The breast is made up of ducts and lobules surrounded by fatty tissue.
- Cancer confined within a duct is called ductal carcinoma in situ (DCIS). Lobular carcinoma in situ (LCIS) is cells confined to a lobule.
- Tumors that break through the wall of the duct or lobule are called infiltrating ductal or infiltrating lobular carcinomas.
TREATING BREAST CANCER
Surgery is the main treatment for breast cancer. This is often followed by radiation therapy to decrease the risk of cancer returning in the breast, chest wall and/or lymph nodes.
Lumpectomy, or partial mastectomy, is the surgical removal of the cancerous tissue along with a small rim of surrounding healthy breast tissue. This type of breast conserving surgery is often followed by radiation therapy.
Mastectomy is the surgical removal of the entire breast. Sometimes, breast reconstruction can be performed after mastectomy. While less common, radiation is sometimes recommended after mastectomy as well.
Both mastectomy and breast conserving therapy (surgery and radiation) can be equally effective approaches in curing breast cancer. Ask your surgeon and radiation oncologist about the risks and benefits of both options.
Radiation Therapy after surgery can decrease the chance of cancer returning in the breast and improve survival. Radiation therapy involves delivering focused radiation to the breast or chest wall, and sometimes the lymph nodes, to treat cancer cells not detected or removed by the surgery. Radiation therapy kills cancer cells by destroying their ability to multiply.
Chemotherapy and/or hormonal therapy are often suggested.
In some cases, chemotherapy may be advised to help keep the cancer from coming back; chemotherapy is usually given before the radiation therapy course.
Sometimes, treatment with a drug to block the effects of estrogen and progesterone also may be suggested.
WHOLE BREAST RADIATION THERAPY

Before beginning treatment, you will be scheduled for a planning session to map out the area of treatment. This procedure is called a simulation. Simulation involves having a CT scan. Tiny tattoo-like marks made on your skin help the radiation therapist precisely position you for daily treatment.
PARTIAL BREAST IRRADIATION
Ongoing research suggests that , for selected patients, it may be safe to give radiation treatment to only the part of the breast that had the tumor, over a shorter period of time
Breast brachytherapy involves placing a balloon, directly into the cavity where the lump was taken out. A small, radioactive seed is guided into the catheters or balloon and is left in place for several minutes based on the treatment plan designed by the radiation oncologist. The procedure is repeated twice daily for a period of five days, then the catheters or balloon are removed and the treatment is finished.
The other available technique is external 3-dimentional conformal partial breast irradiation.
The long-term results of these techniques appear promising but are still being studied. Talk with your radiation oncologist for more information
AFTER MASTECTOMY RADIATION
After a mastectomy, your doctor may suggest radiation therapy for the chest wall and nearby lymph node areas. Whether or not radiation therapy should be used after removal of your breast depends on several factors such as the number of lymph nodes involved, tumor size and whether or not cancer cells were found near the edge of the surgical site.
BREAST RADIATION SIDE EFFECTS
Side effects are usually temporary and usually go away shortly after treatment ends. They may include skin irritation similar to a sunburn, breast swelling , mild tenderness in the breast or chest wall, and mild fatigue that generally gets better a month or two after treatment ends.
During the treatment course you will be seen weekly by your radiation oncologist and a nurse to address these problems.
After the short-term side effects of radiation therapy resolve, others may become noticeable months or years later. These may include breast firmness or mild shrinkage, change in skin color and thickness, sometimes fine blood vessels will appear, scarring of a small part of the lung just under the breast (which may cause a dry cough or shortness of breath that is treatable.) , decrease in the range of arm motion and/or shoulder discomfort.
Hand or arm swelling, called lymphedema, can occur but depends upon the extent of surgery and radiation.
Very rare potential side effects include heart injury for left-sided breast cancers and new tumors caused by radiation. Many factors affect your risk for these side effects. Please talk to your radiation oncologist to learn more about how likely these side effects may be for you.